Join Our eNewsletter!
Subscribe to our monthly newsletter to receive encouraging advice to help you lead a healthy lifestyle.

Osteoarthritis and Rheumatoid Arthritis: How Do They Differ?
According to the Centers for Disease Control and Prevention (CDC), nearly 60 million adults in the U.S. have some form of arthritis. Of the more than 100 types of arthritis, two of the most prevalent are osteoarthritis and rheumatoid arthritis. Osteoarthritis (OA) is the most common type overall, while rheumatoid arthritis (RA) is the most common type of inflammatory arthritis.
What OA and RA Have in Common
The literal meaning of “arthritis” is inflammation of the joints, so osteoarthritis and rheumatoid arthritis both cause similar symptoms, including:
- Joint pain - that can vary in intensity
- Joint stiffness - that can vary in intensity
- Swelling - in the soft tissue around the joint, which typically causes visible puffiness
- Decreased range of motion - that may make walking or performing daily activities difficult
Both types of arthritis are usually diagnosed if these symptoms last three or more days in a row and if several episodes of experiencing the symptoms happen during the course of a month. Doctors may also confirm diagnosis through X-rays or an MRI.
How OA and RA Differ
Although their symptoms can be similar, there are distinct differences between osteoarthritis and rheumatoid arthritis, and each form requires different treatment.
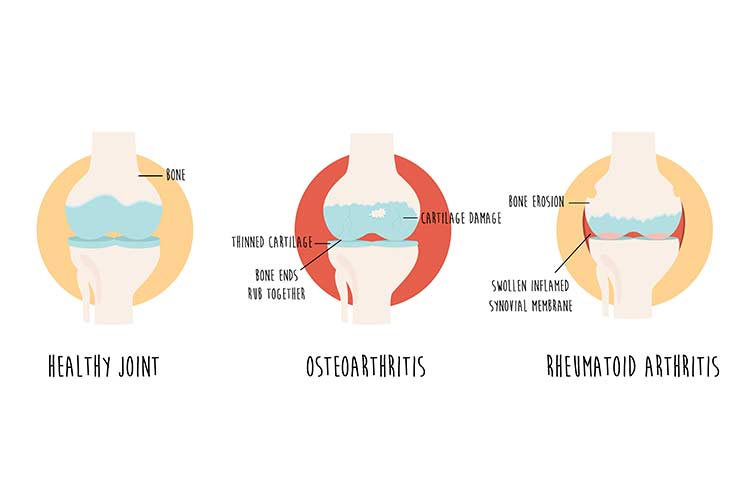
Osteoarthritis
Osteoarthritis is a degenerative disease that causes the entire joint, along with its protective cartilage and fluid, to break down over time. The most common joints affected by osteoarthritis are the knees, hips, hands, and spine. Typically caused by wear and tear, osteoarthritis affects more than 32.5 million people in the U.S., most of whom are over the age of 40.
Symptoms that are specific to osteoarthritis include:
- Pain, stiffness, or swelling that happens gradually and starts in just one joint or one part of the body (such as a hand or knee), as opposed to the entire body
- A grating, popping, or crackling sensation when the affected joint is used, possibly signaling the bones are rubbing against each other
- Bone spurs, extra bits of bone that feel like hard lumps, forming around the affected joint
With osteoarthritis, pain varies from person to person. For some, it can be mild or moderate. For others, it can be unbearable and debilitating. But pain can also vary from day to day, with one day presenting with little to no pain and the next presenting with severe pain.

The symptoms of osteoarthritis can be managed, but the damage caused by the disease can’t be reversed. A treatment plan for osteoarthritis may include one or more of the following:
- Medications, such as acetaminophen, NSAID pain relievers, and duloxetine (Cymbalta)
- Physical therapy or occupational therapy
- Cortisone injections into the affected joints
- Joint replacement surgery in which the damaged joint is removed and replaced with an artificial joint
Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disease, meaning the immune system is malfunctioning and attacking healthy parts of the body. In the case of rheumatoid arthritis, it attacks the synovial membrane that protects the joints. Because it’s a systemic disease, rheumatoid arthritis often affects several joints at once. It can also damage tissue and organs such as the lungs and eyes.
This form of arthritis can begin in people in their 20s and tends to affect women more than men. Rheumatoid arthritis has many physical and social ramifications and can lower quality of life by causing pain, disability, and premature death.

Symptoms of rheumatoid arthritis that differ from those of osteoarthritis include:
- Symmetrical joints are affected, such as both hands or knees or both ankles, at once
- Moderate to severe joint stiffness in the morning
- Joint deformity
- Fever
- Anemia
- Fatigue
- Joints generally feel better with activity
These symptoms may come and go and vary in severity from day to day. Most people with rheumatoid arthritis experience flare-ups followed by periods of remission when the pain and swelling fade or disappear.
Treatment of rheumatoid arthritis may include:
- Medications, such as NSAID pain relievers, corticosteroids, and DMARDs/biologics (drugs that slow the progression of RA)
- Physical or occupational therapy
- Surgical synovectomy, which removes the inflamed lining of the joints
- Surgical repair of the tendons around the joints
- Surgical fusion of the joints
- Total joint replacement surgery
Both osteoarthritis and rheumatoid arthritis can be better managed and potentially cause less damage when diagnosed and treated early. If you suspect you may be experiencing symptoms of arthritis, talk to your doctor.