Join Our eNewsletter!
Subscribe to our monthly newsletter to receive encouraging advice to help you lead a healthy lifestyle.

Nonmelanoma Skin Cancers: Lesser Known, More Common
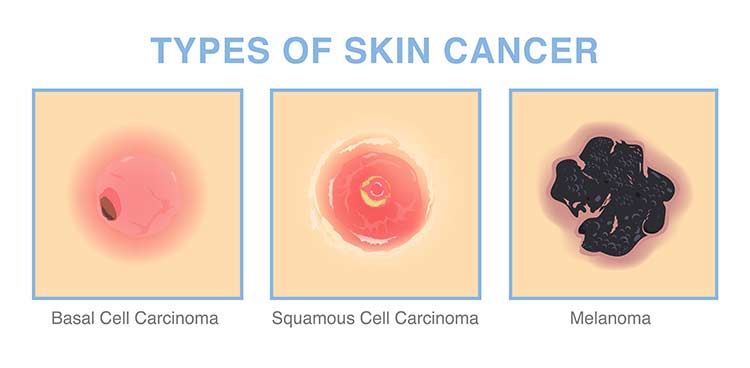
While melanoma is perhaps the most well-known type of skin cancer, nonmelanoma skin cancers are actually far more common. Melanoma is more aggressive than nonmelanoma, meaning it’s more likely to spread to other parts of the body and can spread quickly. But that doesn’t mean nonmelanoma skin cancers aren’t serious.
In fact, more than 5,400 people worldwide die from nonmelanoma skin cancer every month.
The two main types of nonmelanoma skin cancer are basal cell carcinoma and squamous cell carcinoma.
Basal cell carcinoma accounts for up to 80% of all skin cancer cases in the U.S., with an estimated 3.6 million cases diagnosed each year. There are an estimated 1.8 million cases of squamous cell carcinoma diagnosed in the U.S. each year. In comparison, it’s predicted that the number of new melanoma cases diagnosed in 2023 will be 97,610.
What Are the Signs of Basal Cell Carcinoma?
Basal cell carcinoma, the most common form of skin cancer, arises from abnormal, uncontrolled growths developing in the cells of the epidermis, which is the outermost layer of skin.
Most cases of basal cell carcinoma are caused by a combination of intense and long-term exposure to UV rays from the sun. For this reason, most instances of basal cell carcinoma are found on areas of the skin that are regularly exposed to the sun, such as the face, neck, ears, scalp, shoulders, and back.

The appearance of basal cell carcinoma skin lesions varies from person to person and can even look different on one area of the skin than another. Lesions may appear as:
- An open sore that doesn’t heal
- A shiny bump or nodule
- A reddish or irritated patch
- A flat white, yellow, or waxy scar-like area
- A small, slightly raised pink growth with a rolled edge and crusty center
The good news is that basal cell carcinoma rarely spreads beyond the original tumor site, but the lesions can grow wider and go deeper into the skin, potentially destroying skin, tissue, and bone and causing disfigurement. So, it’s important to receive treatment for basal cell carcinoma as early as possible. It’s also more likely that the cancer will recur if you wait too long to get treated for the first occurrence.
There are several treatment options available for basal cell carcinoma, including curettage and electrodesiccation (electrosurgery), Mohs surgery, and excision. Most cases can be treated on an outpatient basis.
How Is Squamous Cell Carcinoma Treated?
The second most common form of skin cancer, squamous cell carcinoma develops in the flat cells located near the surface of the epidermis. Like basal cell carcinoma, squamous cell carcinoma is usually caused by intense or long-term exposure to the sun’s UV rays and is commonly found on the face (especially the lips), neck, ears, hands, scalp, shoulders, and back. But it can also occur in areas of the body that aren’t typically exposed to the sun, such as the genitals.

Also similar to basal cell carcinoma, the appearance of skin lesions caused by squamous cell carcinoma varies person to person. They may appear as:
- A firm, dome-shaped growth, usually red in color
- A red, scaly patch with an irregular border that may crust or bleed
- An elevated growth with a depression in the center that may occasionally bleed and may rapidly become larger
- An open sore that bleeds or crusts and lasts for weeks
- A wart-like growth that crusts and occasionally bleeds
If allowed to grow, squamous cell carcinoma lesions can become invasive, growing into the deeper layers of the skin and even spreading to other parts of the body. So, it’s crucial to receive treatment for squamous cell carcinoma as early as possible.
Squamous cell carcinoma can usually be treated through curettage and electrodesiccation (electrosurgery), Mohs surgery, or excision. If larger lesions are present, radiation therapy may be used.
Prevention and Screening
Since 90% of nonmelanoma skin cancer cases are caused by exposure to UV rays, the best way to reduce your risk is to limit direct exposure to the sun, especially between 10 a.m. and 4 p.m. Avoid sunbathing and don’t use tanning beds or sun lamps.
When you’re outdoors, always wear a broad-spectrum sunscreen that protects against both UVA and UVB radiation and is at least SPF 30. Reapply one ounce of sunscreen every two hours or every hour if you’re in the water or sweating heavily.

You should perform a skin self-exam regularly. Learn the proper way to do it here. If you notice any changes in your skin that may indicate cancer, you should see a Dermatology specialist as soon as possible.
Particularly if you’re high risk because of sun exposure or a family history of skin cancer, you should also be screened by dermatologist once a year.